
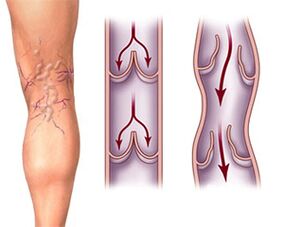
Varicose veins are not only a cosmetic defect that appears on the thighs, legs and upper part of the foot in the form of a blue tree-shaped mesh, accompanied by pain and convulsive spasms in the muscles of the lower leg when walking or exercising, and heaviness. in the legs. First of all, there is a high risk of thrombosis of the inferior vena cava system. It is a serious disease whose symptoms affect one in four people on the planet.
Thrombotic complications provoke the appearance of trophic leg ulcers, acute blood flow pathologies and necrosis of the tissues of the lower extremities. Often, a blood clot that breaks away from the wall of a vessel entering the blood system of the lower extremities ends its journey through the human circulatory system in the heart or brain. The high risk of suffering a stroke or heart attack is the main factor for starting treatment and preventing varicose veins, and not the unsightly appearance of the legs.
Since its beginning, the disease has been constantly progressing, affecting new areas of the internal and external venous system of the legs. Therefore, it would be logical to start analyzing the issue of disease prevention. Competent preventive measures in most cases predetermine the rate of development of pathology, which develops against the background of a hereditary defect in the valvular apparatus of venous blood flow of the legs.
Prevention of varicose veins
The walls of the veins in the lower extremities are very weak, the muscular system is designed in such a way that it cannot help push blood through contractions. To control the directional flow of blood and prevent stagnation, veins have specialized valves. In some people, the valves cannot function properly due to heredity. However, valvular pathology can develop with age due to:
intense physical activity;
increased intra-abdominal pressure;
constipation;
Frequent pregnancies.
Initially, the process develops in the external veins, but as the disease progresses it affects the deep venous network. The process of developing the disease can last decades, and the speed depends on lifestyle, the resistance of blood vessel walls and the intensity of physical activity.
The first task of prevention.– minimize the increase in intra-abdominal pressure, avoid increased overload and combat constipation.
Second task– promote the passive outflow of venous blood from the legs. To do this, there is a technique that must be performed at the end of the day, or better yet several times throughout the day. The essence of the technique is to place your legs extended on the surface at an angle of 45 degrees to the horizontal. You should stay in this position for at least half an hour. For those people who already suffer from varicose veins, it is recommended to sleep with your legs elevated as often as possible.
If you have a disease, you should not wear tight shoes or socks with a tight elastic band, so as not to complicate the already impaired blood circulation.
In addition, when doing sedentary work or simply sitting for a long time, you should try to keep your legs in a horizontal position and, if possible, place them in elevation. Naturally, this does not mean that when working in an office you should sit with your feet on the table. No. Just try putting something under the table that allows you to rest your feet unobstructed while sitting. You should also avoid the habit of crossing your legs while sitting. At home you can elevate your legs by placing several cushions.
Conservative treatment
The non-surgical treatment program consists of diet, medication and compression therapy.
Diet
One of the risk factors for developing varicose veins is excess weight. Therefore, diet is one of the factors of treatment. Nutrition must be balanced so that the calories received do not exceed the amount necessary to cover daily needs. Additionally, the number of calories varies depending on the presence or absence of exercise. You should also eliminate spicy seasonings, marinade, pepper, excess salt, alcohol, smoked foods from your diet, and also eat less fried foods.
The menu should consist of a sufficient amount of vegetables and fruits containing vitamin C, dishes containing a large amount of fiber, seafood and whole grain bread. Small, frequent meals are recommended. It is important to note that animal fats should be present in moderation. You should not listen to those who say that cholesterol is an absolute evil. Cholesterol in reasonable amounts helps strengthen vascular walls, reducing the risk of venous ruptures and recurrent thrombotic deposits.
Give up smoking
Smoking tobacco is the most harmful habit for varicose veins. The fact is that the tars contained in cigarettes clog blood vessels, and carbon dioxide causes vascular spasms. Smoking increases the risk of blood clots and, as a result, secondary complications such as heart attacks and strokes. Smoking is especially dangerous for those who, having varicose veins, take hormonal medications.
Compression underwear (tights, stockings, knee socks)
This prevention and treatment option is very suitable in the early stages of the disease. Lingerie can be selected based on various parameters of pressure on soft tissues, color combination and model option. The underwear is put on in the morning, without getting out of bed, until the veins overflow with blood. The main obstacle to the use of this prevention method is the inflated price. Therefore, the main consumers of knitwear are not those who need prevention, but those who, after surgery, use underwear for secondary prevention purposes.
Varicose veins: treatment with medications
Medicines cannot completely cure or stop the disease.
Venotonics – ointments and gels

Venotonics aim to strengthen the walls of the veins, stimulate blood flow and slightly improve microcirculation. These medications, when taken together, can reduce pain and swelling. The course of use of the drug is carried out twice a year and lasts at least two months.
Ointments and gels, although safe, are practically useless. They cannot penetrate beyond the skin and therefore affect the state of the blood vessels. Ointments and gels are prescribed in the early stages of the disease, when it is not yet known what can relieve swelling and heaviness in the legs: medications or postural drainage and cessation of physical activity. Sometimes ointment manufacturers are cunning and recommend using the product in combination with tablets.
ointment based on rutin flavonoids.
An ointment containing horse chestnut extract is applied twice a day.
gel, whose active ingredient is an extract of grape leaves. There are also capsules of the medication that are taken on an empty stomach twice a day.
Venotonics in tablets.
Venotonics in tablets are used for varicose veins.
Saponin derivatives of the drug are obtained on the basis of horse chestnut, which contains the plant bioflavonoid escin. These include the drug, which exists in the form of drops and dragees.
The most effective preparations are made from a plant flavonoid obtained from citrus fruits, a powerful venotonic. The course of treatment with these drugs can last up to six months.
Rutosides are the first venotonics. Its effect is to improve microcirculation and have an anti-inflammatory effect.
Natural rutoside, which is available in the form of tablets and capsules.
Semisynthetic rutosides.
Combined rutoside. Combines a semi-synthetic derivative of rutin and ginkgo biloba extract. The medicine in the form of capsules is taken twice a day for a month.
Phlebosclerosing medications
Allows you to exclude veins from the bloodstream without surgery. The action is achieved by the growth of connective tissue, which gradually closes the lumen of the vessel. The connective tissue is stimulated by increased coagulation of endothelial proteins, as well as by irritation of the smooth muscles of the vessel.
The simplest option is an ointment based on glycosaminoglycans, glucocorticoids and nonionic surfactants containing acid sulfur. However, the effect is so weak that injectable solutions are used.
Synthetic phlebosclerotics.
Products containing iodine or based on animal proteins. Medications are used to selectively close small vessels in affected areas of the veins. Among doctors, drugs that do not cause vascular thrombosis are popular.
 They only burn the walls at the endothelial level.
They only burn the walls at the endothelial level.
Phlebosclerotic therapy involves injections of medications or elastic bandages. It is a fairly simple, painless technique that does not affect the patient's well-being and is very popular among doctors.
However, sclerotherapy alone does not provide lasting results and cannot stop disease progression. Therefore, it is best to use it in combination with surgical treatment. Before therapy, it is necessary to undergo ultrasound of the lower extremities to exclude extensive lesions of the saphenous and deep veins.
Contraindications for phlebosclerosis are: drug allergies, atherosclerosis of the large vessels and the presence of ischemia, obliterans endarteritis, diabetic angiopathy, damage to the blood coagulation system, pregnancy, acute thrombophlebitis of the legs.
Additional medications
Agents that improve blood microcirculation: low molecular weight dextrans, derived from purine. These medications stimulate the breakdown of platelets, reduce blood viscosity, and increase the elasticity of red blood cells. These processes improve blood supply to tissues and oxidative reactions in them.
Anticoagulants of direct or indirect action. Reduce the risk of thrombosis. Popular products in the form of ointments and gels have antiedematous, anti-inflammatory and antithrombotic effects.
Non-steroidal anti-inflammatory drugs - suppress inflammatory processes and relieve pain.
Phlebosclerosant therapy options
Before surgery, venous sclerosis is performed to reduce the risk of thrombosis and bleeding in the postoperative period.
During surgery as an alternative to vein removal.
After surgery to close unoperated veins.
The puncture method of administering medications is used at any time and the catheter method is used exclusively during surgery.
puncture method
In addition to the operating room, it can only be performed in a specialized operating room respecting all aseptic standards. The large veins are closed first and then the small ones. Medications are administered from top to bottom. The vein is punctured with the patient in an upright position and medications are administered in a horizontal position. If sclerosis of a dilated vessel is necessary, the procedure is performed in several sessions. After the sessions, the patient is registered with a phlebologist for three years for observation.
After administering the drug, the limb is subjected to elastic bandage, which is repeated for two weeks. During the first week, the bandage is not removed.
The patient should walk within half an hour after the procedure.
The patient should sleep with the extremities elevated every day and avoid sitting or standing for long periods of time, as well as walking a lot.
Radiofrequency ablation of veins.
Vein ablation using a radiofrequency emitter is a recently emerging area of phlebology. This method allows you to get rid of varicose veins without pain, without complications and with minimal risk of vascular injury. Radiofrequency radiation acts on the inner lining of the vascular wall and destroys it. Therefore, the lumen of the vein collapses, and neighboring tissues are practically not affected. This is a very effective method.
The procedure is performed under local anesthesia on an outpatient basis. For greater precision during the procedure, monitoring is performed using duplex angioscanning.
Once the anesthetics have taken effect, a venipuncture is performed. A catheter with an emitter is inserted into the vein. It advances to the point where the saphenous vein joins the deep venous system. With gradual withdrawal of the catheter, sequential irradiation of the vessel from the inside occurs. After the procedure, the puncture site is treated and covered with a bandage. A special elastic stocking is placed on the leg. After half an hour of walking under supervision, the patient is allowed to go home. If the patient's job does not involve physical labor, she has the right to work the day after the procedure.
Varicoseextensionveins: operation
The appropriateness of surgical intervention is considered by a phlebologist or vascular surgeon. For women who need surgery to correct a cosmetic defect, doctors suggest postponing surgery if they are planning a pregnancy. This is due to the fact that during pregnancy varicose veins progress and the effect of the operation can be neutralized.
combined phlebectomy
The most common option to solve the problem of varicose veins through surgery is combined phlebectomy. The surgery is performed under general anesthesia or local anesthesia. All incisions are made as small as possible. For example, the great saphenous vein is removed through a one and a half centimeter incision in the groin area. A phlebextraction tube with a special tip is inserted into the vein through the incision. After this, the tube is removed along with the vein. Small veins are removed through small tubes, called a miniphlebectomy. After surgery, compression garments should be worn.
Endovasal electrocoagulation
Removal of saphenous veins by current. A more dangerous method compared to radiofrequency obliteration and classical surgery.
cryosurgery
Removal of veins through exposure to low temperatures. The method is relatively safe. True, the depth of freezing is not always accurately calculated, leading to damage to adjacent tissues or incomplete removal of the vein.
Intraoperative scleroobliteration
The use of catheter injection of a sclerosing agent into the saphenous veins. Before leg surgery, the saphenous veins and altered areas of the veins are marked. During the operation, the anastomosis of the great saphenous vein and the femoral vein is exposed. The tributaries of the great saphenous vein are ligated. At a distance of 1 centimeter from the femoral vein, the saphenous vein is crossed and ligated. A catheter is inserted into the cut vein, the vein is sutured, and the wound is dressed. A roll of gauze is placed along the projection of the saphenous vein along the entire leg and pressed. Simultaneously with the removal of the catheter, a sclerosing agent is injected.
endoscopic dissection
Transillumination phlebectomy of perforator veins allows the veins to be ligated and excluded from the bloodstream. These veins connect the subcutaneous network of veins with the deep network. An endoscopic probe is used.
Laser coagulation
The vein is sealed from the inside with a laser and excluded from the bloodstream. It requires a highly qualified doctor and sufficient experience working with lasers.
Home treatment for varicose veins.
At home, varicose veins can be treated with pills, rubbing ointments, leeches, apple cider vinegar and cabbage leaves. Home treatment can also be performed by using compression garments or elastic bandages. But if the disease is advanced, none of the methods will help without surgical treatment.
Today, the only high-quality way to get rid of varicose veins is surgical methods, as well as cases of combining surgery with sclerotherapy and compression methods.

















